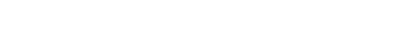
A Four-Pillar Program to Preserve Brain Health
Posted in News | Tagged 4 pillars, action, alzheimers, brain health, brigid reynolds, dementia, emotional health, four pillars, kathleen johnson, knowledge, margaret bassett, melanie chadwick, memory disorders program, physical health, preserve brain health, scott turner
R. Scott Turner, MD, PhD, Brigid Reynolds, NP, Kathleen Johnson, NP, Melanie Chadwick, NP, Margaret Bassett, NP, and the Memory Disorders Program
PILLAR 1: MAINTAIN PHYSICAL HEALTH
Participate in regular exercise.
Three to five sessions per week and at least 30 minutes per session. Complete both resistance and aerobic exercises – intense enough to break a sweat and increase pulse to the recommended range (roughly 220 minus age), and intense enough to preclude having a casual conversation. But first, clear any exercise program with your primary care provider or cardiologist. Consider consulting or hiring a personal trainer to increase compliance.
Consume a Mediterranean diet.
This consists primarily of fruits and vegetables, fish, nuts, beans, olive oil, and red wine in moderation. This mostly plant-based diet should be high in fiber and low in total calories, simple sugars (glucose, fructose, sucrose), salt, saturated fats, trans-fats, cholesterol, red meat, and processed foods. Consume liquid vegetable fats (e.g. olive oil) and avoid animal fats (e.g. butter). Avoid consuming all solid fats (coconut oil, palm oil). Discuss dietary changes with your primary care provider. Consider consulting a nutritionist to increase compliance. For more information, go to www.heart.org.
Maintain Ideal body weight – throughout life.
This will naturally follow from the two points above. Obesity, particularly during midlife, increases risk of diabetes, mild cognitive impairment (MCI), and Alzheimer’s disease (AD). Use intermittent fasting if this helps maintain ideal body weight. Lose weight if overweight or obese. Consider medications if needed (or bariatric surgery for morbid obesity).
No smoking.
No tobacco or other inhaled products.
Limit alcohol.
One serving per day for women and one-two servings per day for men (or no alcohol at all if these limits cannot be maintained). One serving is 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirit.
Strive for adequate sleep.
About 7-8 hours per night is adequate for most individuals. A 30-minute nap in the early afternoon is acceptable if needed. Maintain good sleep hygiene (avoid caffeine and other stimulants after midday, etc.). Avoid long-acting sleeping pills with the potential for cognitive side-effects.
Avoid traumatic brain injuries.
For younger individuals this means using seatbelts and helmets. Avoid boxing and other contact sports with a high risk of concussion. Use fall prevention strategies for older individuals (declutter, remove area rugs, etc.). Physical therapy may improve balance and strength, and reduce fall risk in individuals with poor conditioning or orthopedic problems. Use walking aids if recommended to prevent falls.
Consider taking a daily multivitamin.
To date, no supplement or medical food has proven benefits in preventing or treating cognitive decline or dementia. A daily multivitamin (with recommended daily allowances) may ensure adequate vitamin D and vitamin B12 levels.
Use eyeglasses and hearing aids if needed.
Do not deprive your brain of sensory input. Have your vision and hearing tested if needed.
Maintain dental hygiene.
Keep regular appointments with your dentist and dental hygienist. Chronic inflammation – such as gingivitis – increases risk of dementia.
Monitor and treat hypertension.
Take medications if needed.
Monitor and treat diabetes and pre-diabetes.
Diabetes may be prevented, delayed, or perhaps even reversed by following the first three points. Take medications if needed to control blood glucose, and monitor their effectiveness daily (blood glucose monitoring) and long-term (HgbA1c level) with your primary care provider or endocrinologist.
Monitor and treat high cholesterol.
Take medications if needed.
Monitor and treat obstructive sleep apnea.
If needed, use devices as instructed to assist with breathing during sleep (such as continuous positive airway pressure (CPAP)).
Prevent and treat sexually transmitted diseases.
HIV and syphilis are readily preventable and treatable.
PILLAR 2: MAINTAIN EMOTIONAL HEALTH
Minimize stress.
Identify and remove or minimize sources of anxiety. Forgive and let go of grudges and feuds – or move on. Simplify and minimize where possible. Clutter causes anxiety – keep only things that “spark joy.” Simplify and consolidate finances. If there are specific instructions regarding assets in your will consider acting on these now – before death – if this is a concern. Keep legal affairs in order (including advance directives). An active spiritual life brings peace to many. Caring for a pet may be of benefit. Find purpose and meaning in life – consider volunteering or working part-time.
Monitor and treat depression and anxiety.
Take medications if needed, but avoid medications that may interfere with memory. Depression and anxiety adversely impact memory, and if treated may lead to recovery. However, depression and anxiety may be the first sign of dementia.
Engage in cognitive and mental activities.
A higher quantity and quality of education is protective (resilience). Brain games on your desktop, laptop, tablet, or cellphone with apps such as Lumosity (lumosity.com) and BrainHQ (brainhq.com) may be helpful. Maintain hobbies and activities that engage the brain. Seek new hobbies and activities. Limit television to 1-2 hours per day.
Participate in social activities. Social connections and activities are important. Maintain old connections and seek new ones – not just online but in person.
PILLAR 3: KNOWLEDGE
Be knowledgeable about your health and personal risk.
Consider home-based genetic testing. Companies such as 23andMe (23andme.com) test for disease risk genes including ApoE4 – a normal variant of ApoE. This is not a diagnostic test. ApoE4 increases risk of AD, but many patients with ApoE4 do not develop AD, and of patients with late-onset AD, about 40% are negative for ApoE4. Secure all desired insurance policies BEFORE genetic testing – health, life, disability, and long-term care – due to the possibility of insurance discrimination post-testing. Keep genetic testing results confidential as they also have implications for family members (parents, siblings, and children).
PILLAR 4: TAKE ACTION
Seek evaluation and treatment if memory problems develop.
This includes screening for hypertension, diabetes, high cholesterol, sleep apnea, depression/anxiety, and medications that may impair memory (prescription and over-the-counter). Test for thyroid dysfunction, vitamin B12 deficiency, HIV, and syphilis if indicated. Consider FDA-approved treatments for individuals diagnosed with dementia due to AD. To date, four medications (in two different classes) have proven safety and effectiveness, and are routinely prescribed. These medications are well-tolerated by most individuals. These drugs should not be prescribed for healthy normal individuals or those with MCI – due to lack of effectiveness.
Learn about research options in your area.
Consider joining a study. The clinicaltrials.gov website is searchable by geographic area and diagnosis. Research may entail further diagnostic tests (otherwise unavailable), and a new treatment (versus placebo). Individuals do not pay to participate in studies; they receive no bills, and study procedures they undergo are covered by the study sponsor, not their insurance company. The APT webstudy (aptwebstudy.org) is one example – this is a confidential memory test conducted at home. Repeated testing tracks cognitive performance over time (months-years) – at no charge.
IN CONCLUSION
Following this Four-Pillar Program
Following this Four-Pillar Program may delay the onset, slow down, or prevent dementia and AD by 5-10 years. But if all pillars are followed, life expectancy may also increase by 5-10 years, and the #1 risk factor for cognitive decline and dementia is aging. However, compliance will restore balance and maintain cognitive performance with aging. Adhering to only part of the Program may be less effective or ineffective. The goal is to maximize health-span and lifespan while minimizing years of disability (cognitive and/or physical) at end-of-life.
THE MEMORY DISORDERS PROGRAM
We provide clinical care and management for older individuals with memory loss, MCI, and AD – with a primary focus on research. Our clinical services include:
- Taking a medical history, performing a physical examination (including neurologic and cognitive assessments), reviewing medications, and ordering blood tests and a brain imaging study (MRI or CT scan) if indicated.
- Ordering optional diagnostic tests including additional blood tests, genetic testing, spinal fluid analyses, neuropsychologic testing, electroencephalogram (EEG), polysomnogram (sleep study), vision testing, hearing assessment, and brain imaging (a glucose PET scan).
- Providing a specific diagnosis of cognitive dysfunction or dementia in order to determine prognosis and further management. Dementia is not a diagnosis – and has many causes. Dementia is a decline in memory and other cognitive abilities due to an underlying disease. Dementia may be caused by AD, Lewy body dementia, frontotemporal dementia, multiple strokes, HIV, traumatic brain injury, chronic alcoholism, and other disorders – or a combination of these (mixed dementia).
- Prescribing medications (if indicated) in addition to discussing non-drug therapeutic strategies. FDA-approved medications may stabilize or slow down cognitive and functional decline. Other medications may address specific behavioral issues including depression, anxiety, apathy, agitation, delusions, hallucinations, and circadian (sleep) disturbances.
- Providing appropriate consults and referrals to other medical providers and local agencies including the Alzheimer’s Association (alz.org). We may provide a referral to a Social Worker or Care Manager for advice and recommendations on assisted living and nursing home options in your area.
- Referring to speech therapy, occupational therapy, and/or physical therapy if indicated.
- Providing counseling and education to the patient, family, and caregivers. This step alone minimizes emergency room visits and hospital admissions for individuals with dementia.
- Providing our contact information for follow-up questions and issues as they arise and dementia progresses.
- Providing medical documentation essential for short-term or long-term medical leave, disability insurance, and other legal affairs (including exclusion from jury duty).
- Providing specific recommendations regarding supervision of activities of daily living (driving an automobile, managing household finances, and taking medications correctly) depending on dementia stage.
Our Program’s Focus
Our program’s focus is on research, and due to that emphasis our clinic time is limited. Therefore, the option of research participation may be discussed with individuals and study partners who are interested and eligible for studies. In fact, we prioritize clinic appointments for individuals who are interested and eligible – or who may become interested and eligible – in research. For those seeking clarification of diagnosis, we may schedule a one-time diagnostic consultation only. We typically refer to private practice providers if an individual is neither eligible nor interested in research.
About Our Research
We provide a menu of research options – these may require only one visit with no investigational treatment (biomarker discovery and validation), or may involve many visits over one or more years evaluating a new treatment (versus a placebo). Research studies may include blood tests, genetic testing (including ApoE), functional MRI, spinal fluid analyses, amyloid, tau, and glucose-PET scans of the brain, and additional study-specific tests. We also offer the possibility of brain donation after death – this provides a definitive diagnosis and contributes to research. Our studies, including those seeking volunteers and study partners, are listed at memory.georgetown.edu. Referral to other research sites in the area may also be offered.
Science-based Care
The Memory Disorders Program at Georgetown University is a nonprofit organization. We do not order unnecessary diagnostic tests and we do not advertise or sell unproven supplements, medical foods, devices, and other putative cures. To date, no supplement, medical food, or device has proven safety and effectiveness to prevent or treat dementia. As we gather additional data regarding the Four-Pillar Program, we practice only evidence-based medicine.
Our research studies adhere to the highest scientific standards in order to make progress in the field of dementia, and AD. We discourage the use of costly, unproven, and unnecessary medical tests and supplements, medical foods, and devices outside of research, but recognize that while costly they are generally recognized as safe in healthy young individuals. There is inadequate research on supplements, medical foods, and devices to know their effects on health and their potential interactions with other medications. Due to lack of regulation, there is no guarantee regarding the content and purity of supplements and medical foods on the market.
Our ultimate goal is a world without dementia due to AD, and we welcome your contribution and participation towards achieving this goal.
References:
- Saif N, Sadek G, Bellara S, Hristov H, Isaacson RS. Brain health and dementia risk reduction. Practical Neurology, 89-94, 2019.
- Rabin JS, Klein H, Kirn DR, Schultz AP, et al. Associations of physical activity and beta-amyloid with longitudinal cognition and neurodegeneration in clinicallyl normal older adults. JAMA Neurology, published online 16 July 2019.
- Kivipelto M, Mangialasche F, Ngandu T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer’s disease. Nature Reviews Neurology 14:653-666, 2018.
- Brasure M, Priyanka D, Davlia H, Nelson V. et al. Physical activity interventions in preventing cognitive decline and Alzheimer-type dementia: A systematic review. Annals of Internal Medicine 168:30-38, 2018.
- Kane RL, Butler M, Fink HA, Basure M, et al. Interventions to prevent age-related cognitive decline, mild cognitive impairment, and clinical Alzheimer’s-type dementia. Comparative effectiveness review no. 188. AHRQ Publication No. 17-EHC008-EF. Rockville, MD. Agency for Healthcare Research and Quality, 2017.
30 August 2019